Creating the first set of effort independent pulmonary diagnostics for airflow, nose-mouth distribution, and natural breathing behaviors for children and infants
A significant portion of our impact evaluation and analysis is based on discovering bed-side problems frequently encountered by technicians, technicians, respiratory therapists, pulmonologists, and neonatalogists. Innovations in breathing analysis, new procedures, and common problems all stem from observations obtained through a significant number of in-person interviews we have conducted that lead to the discovery of difficult and unsolved problems in pediatric and neonatal respiratory monitoring. Our aim is to provide the first respiratory diagnostic system that provides meaningful quantitative metrics and insight to help improve care quality and patient outcomes.
Pediatric Impact
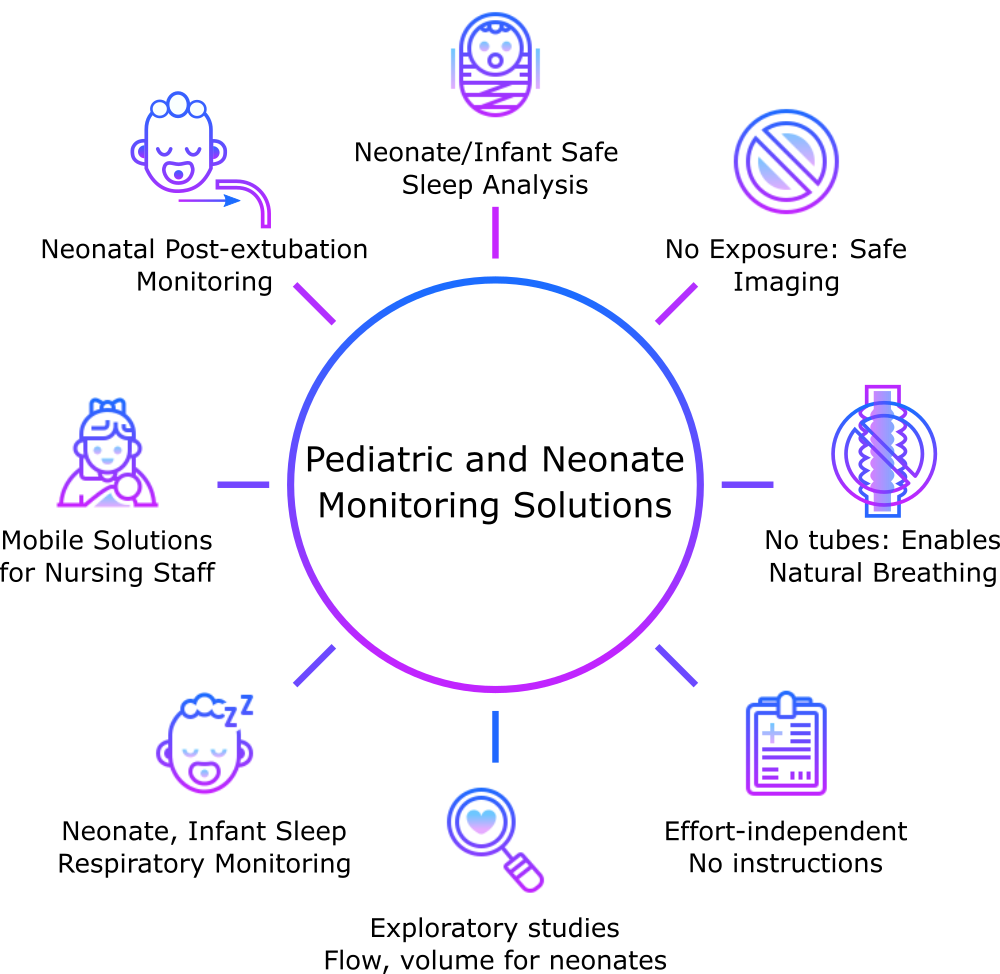
Respiratory health plays an important role in early life development and can have considerable implications for children including poor school performance, cognitive function, and even changes in facial development due to how natural breathing habits are formed. With current solutions available to continuously monitor breathing behaviors, many of them are not well suited for use with children. This may be due to any extended duration of breathing through a tube which quickly becomes uncomfortable, trying to provide precise instructions for how to complete specific tests (peak flow, forceful blowing) which all depend on the child’s performance meaning that they will be effort dependent measurements. To simplify this process, visual analysis of exhale behaviors provides a method that can be used with small children by simply watching their breathing behaviors passively. This ensures that behaviors are captured during a longer monitoring duration and are not inhibited by tubes or other devices, providing insight into how they normally breathe in their everyday life.
Neonatal Impact
Respiratory disorders are the leading cause of early neonatal mortality (0–7 days of age), with the American Academy of Pediatrics reporting that 10% of neonates will require assisted breathing during this period [1]. Being able to identify respiratory health, behaviors, and when to employ certain life saving procedures is a complex process in the Neonatal Intensive Care Unit (NICU). Continuous respiratory monitoring of infants and neonates is extremely difficult without the use of ventilators or assistive breathing devices. Even in the instances where some respiratory information can be obtained using other monitoring techniques such as imaging or respiratory belts alone, the only reliable quantitative metric that can be obtained in a non-contact method is breathing rate as Breathes Per Minute (BPM) or Respiratory Rate (RR). While this metric is important, our aim is to enable a vast number of additional metrics that can be used to diagnose complex breathing conditions in neonates. This includes the ability to observe natural breathing behaviors, continuously monitor high-risk neonates for physiological abnormalities, and introduce the first method to remotely measure airflow and volume of unassisted neonatal breathing. In addition to opening the door for these new metrics, we also focus on several neonate-specific challenges that can be assisted through our new form of respiratory analysis.